Elected leaders joined regional healthcare executives, nonprofit providers, and public health and treatment services staff last week for the first time to convene a Tri-County policy summit on opioids, which claimed the lives of at least 180 people in the region last year.
“We are in a deep, deep hole that we need to climb out of,” said Dwight Holton, chief executive officer of Lines for Life and emcee for the event. “It’s unprecedented to get a power structure of this size, representatives from half the state, in a room at once to look at policy changes.”
Commissioners from Multnomah, Washington and Clackamas Counties were joined by district attorneys and sheriffs, staff from county health and human services divisions, nonprofit treatment providers, regional hospital systems, health insurers and first responders. The six-hour summit, held Friday, April 13, at Marylhurst University, focused on intersections between public safety, treatment and housing — and offered solutions and stories of hope.
[View photos from the 2018 Tri-County Opioid Summit]
Multnomah County Commissioner Lori Stegmann said she was grateful that experts from different sectors came together to propose recommendations. “It’s really about making an ecosystem around housing, addiction treatment and mental health services,” she said.
Addiction is a Chronic Disease
“The history of drug policy in America has not been successful and appears to be driven by racial bias; and that problem persists for generations as mass incarceration,” Tri-County Health Officer Dr. Paul Lewis said in opening remarks. “We have to acknowledge that and try to do it better in this moment, when we’re in a position to implement things.”
After years of holding the line of opioid overdose deaths, the number of deaths began to rise three years ago, largely due to the synthetic opioid fentanyl. At least 47 people died from the drug in 2017, three times the number of deaths from just a year earlier. Emergency departments log more than 1,000 visits each year due to drug overdoses, while 4,500 people enter drug detox centers. While opioid prescription rates have declined, doctors are still handing them out to more than 120,000 Tri-County residents every three months. Meanwhile, a typical dose of heroin costs $10, and a dose of fentanyl costs just $4.
But there’s reason to be hopeful, Lewis said. Multnomah County and nonprofit service provider Outside In continue to exchange used syringes for clean ones, protecting people who inject drugs from deadly infections and viruses. They collected more than 5 million syringes in 2017, and trained 4,500 people on how to administer naloxone, a drug that reverses the effects of a drug overdose. The agencies have received nearly 3,000 reports of rescues because of the drug.
“Imagine what our [drug-related death] rates would be like without that effort,” Lewis said. He called on policymakers and the healthcare industry to view addiction as a disease.
“This is a chronic disease and chronic diseases don’t leave you,” he said. Like asthma, diabetes or hypertension, addiction has genetic and environmental factors. And like other diseases it can often require medication to treat effectively. For people addicted to opioids, treatment that includes medication is more effective at staving off a relapse.
Tim Hartnett, executive director of the treatment provider CODA, thanked Lewis for focusing on medication-assisted treatment. “Medicine is the single best thing we know works for people who have an opioid dependence,” he said. “It’s not the sole cure. But we know it’s absolutely one of the crucial resources to help people.”
He asked policymakers to expand access to that treatment in county jails. CODA providers services in partnership with Multnomah County Corrections.
“Jail is an entry point on that path to recovery,” he said. “Help them respond to the alcohol and drug use that’s right in front of them.”
Prosecution Diversions and Jail-based Treatment
Multnomah County Sheriff Mike Reese said he’s working with his deputies, both on patrol and in county jails, to keep people from coming back to jail when their criminal conduct is largely driven by addiction. His jails book 35,000 people each year, and most are released almost immediately. The average stay is 12 days, and his deputies see many of the same faces over and over again.
“There are a lot of people who just churn through the system,” Reese said. He said recovery can start with a simple conversation, in which his staff see those inmates as having an illness instead of just as criminals.
“We can have a profound impact on people in our custody by treating them with dignity and respect,” he said. “You can turn people's lives around, help them to feel self worth, by showing them human dignity, and still holding them accountable.”
That’s what happened to Niko, 22. He started using drugs in his early teens and escalated from marijuana to cocaine, then to prescription painkillers, heroin and methamphetamines. He tried to stop. He even enrolled in military school and stayed clean for six months. But when he got out, he relapsed.
“I couldn’t figure out how to cope with what I was doing to myself. I knew I needed to stop. I would tell myself, ‘I can’t continue this tomorrow.’ And in the morning, withdrawals would take over and I’d be right back,” he said.
He had run-ins with law enforcement and racked up a series of convictions for possessing a controlled substance. It didn’t stop him.
“I lost the willingness to live,” he said. “I didn’t care if I wasn’t going to wake up.”
Friends died. One man overdosed on a pill that looked like oxycontin but was in fact fentanyl. Another man died from an overdose in Niko’s house. When police responded, a Clackamas County deputy sat down and talked to Niko for about an hour.
"He told me, ‘The guy who died, you don't have to be him. You don’t have to die,’" Niko recalled. "I had heard this from my family. But coming from someone in a position of power, to express some faith in me, allowed me to believe in myself for once."
Now, 10 months clean, he’s enrolled in community college. “I have goals and a purpose in life. I needed to feel I could believe in myself.”
Niko got clean with help from Clackamas County Corrections’ Substance Abuse Program, in which inmates begin a 12- to 18-month treatment program that transitions from the jail to a community-based center across the street. Clackamas is the only county in the state with a drug and alcohol treatment program that also included medication for those recovering from addiction to opioids.
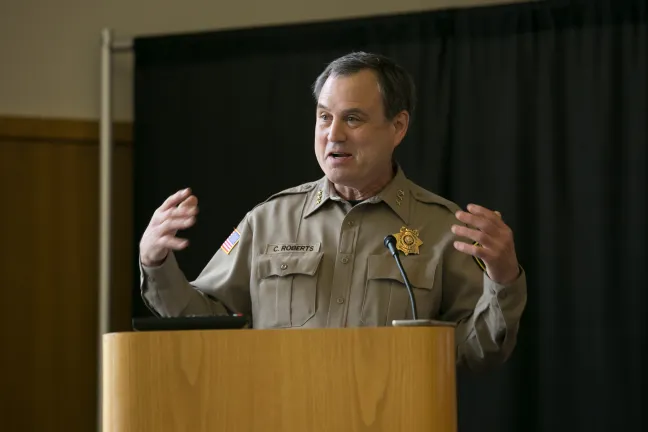
“There’s an opportunity when they’re in our jail,” said Clackamas County Sheriff Craig Roberts. Once an inmate is ready to move from the jail, an employee walks with that person to the transition center, where a team helps coordinate ongoing treatment, mental health services, GED classes, job skills, sober housing and physical healthcare. Periodically the sheriff invites the deputies who arrested the inmates to visit with them and see their progress.
“You can’t believe the change in our patrol, when they interact with clients,” he said.
Multnomah County District Attorney Rod Underhill said his office has also begun shifting to a “treatment first” model. Defendants charged with misdemeanor drug offenses might be candidates for treatment, and eligible to have those charges dropped if they succeed. Others charged with a drug-related felony could see that charge reduced to a misdemeanor. And last year, Underhill’s office adopted a Seattle-based pilot program called LEAD, or Law Enforcement Assisted Diversion. Focused in Portland's downtown core, the program diverts some people who would normally be arrested for low-level drug-related offenses from jail to treatment before they’re even charged with a crime.
"Historically we know enforcement of drug laws has disproportionately impacted people of color," Underhill said. "We have endeavored to overhaul our response. In the last year and a half, we have adopted a different approach. The theme is treatment first. We want to take a step back and make space for a different approach."
Multnomah County Commissioner Jessica Vega Pederson said she appreciates law enforcement’s willingness to examine -- and then address -- the underlying causes of crime.
“There’s a tension between holding people accountable for their behavior and treating the underlying causes of that behavior,” Multnomah County Commissioner Jessica Vega Pederson said. “This really drove home the need for coordination between different governments and law enforcement and with healthcare systems."
More from First Responders and Emergency Departments
Jackie Robinson overdosed on heroin in his Clackamas County home, he told those gathered for the summit. Someone called 911, and he was treated and released. He went home. But a few days later. the firefighter who had saved Robinson’s life was back outside Robinson’s place, knocking on his door to find out if he wanted to get into treatment.
“It was shocking,” he said. “I didn’t expect anyone to come look and see about helping me. I didn’t have insurance. It was hard to seek treatment.”
The paramedics helped connect him with recovery housing — shared housing where people abstain from alcohol and drugs and which often incorporates treatment and meetings of Alcoholics Anonymous and Narcotics Anonymous. Amy Jo Cook, a first responder with the Clackamas Fire District, said the Community Paramedic Overdose Response program started as a way for first responders to play a more active role in fighting the opioid epidemic.
“I’ve been on hundreds, if not thousands, of calls for opioid overdose. We go. We administer naloxone. We put them on a cot and send them to the hospital,” she said. “Inevitably we come across the same person again. we give them naloxone, we put them on a cot, we take them to the hospital. Unless something breaks that cycle. And a lot of times death breaks that cycle.”
Now those same paramedics go out and find the people they’ve saved — sometimes in their homes or apartments, but often in camp sites — and help them navigate a system of treatment and healthcare in hopes that they won’t need to be saved again.
Every time Cook takes someone into the emergency department because of a drug overdose, that person’s life expectancy drops precipitously, research shows. A person who comes in because of an overdose is five to 50 times more likely than a member of the general public to die within the next 10 years, said Jeremy Lynn, an emergency room doctor and director of emergency services for Oregon’s Providence Health and Services.
Compare that to a person who admitted to an emergency department after a heart attack. That person is just twice as likely as a member of the general public to die in the next 10 years. That’s in part because the medical community hasn’t always viewed addiction as a chronic disease, meaning it’s just begun investing in wrap-around services to treat those patients once they leave that intensive care.
Nearly a decade ago, Lynn said, a patient came to the emergency department with a bloody arm. The man said his arm was crushed while he was moving a refrigerator. But then, Lynn recalled, a nurse told the man she had seen him the day before at another emergency department. It turned out the man had cut himself near the site of an old fracture in order to obtain painkillers.
“We were like, ‘Ah ha! Gotcha!’ We kicked him out and were high-fiving,” Lynn said during the summit. He told his wife the story that night. A psychiatrist, Lynn’s wife was less enthusiastic. “‘That’s great, Jeremy,’” he recalled her telling him. “‘But what did you do for his addiction? The main thing he came in for?’ That’s the medical condition that we failed to diagnose."
Emergency departments can do more, Lynn said. They can initiate medication and shepherd patients into treatment programs -- but only if they have program partners and only if those programs have the capacity to do the work.
Alex Baumler, Lines for Line director of operations, said technology can foster that kind of coordination. He proposed a central clearing house that shows, in real time, open spaces at residential and outpatient treatment facilities. “We have individuals who want and need treatment. And we have treatment,” he said. “But often we don’t connect the two.”
The average amount time someone can last on a waitlist before relapsing is 30 days, he said. But having to wait that long cuts by half the likelihood that someone will complete even four sessions of treatment.
“The bottom line is delaying access to treatment leads to worse outcomes,” he said.
Multnomah County Commissioner Sharon Meieran, who works as an emergency room doctor, can relate to Lynn. She used to react the same way when people came in, seeking drugs.
“You knew they were lying to you,” she said. And among those who came in because of an overdose, many were combative. They might spit at her or call her vulgar names.
“They were not very nice, and we were not very nice back,” she said. Her reaction changed once she looked at addiction as a chronic relapsing disease and saw someone with an addiction the way she saw someone with congestive heart failure. Today she is kinder, more compassionate. She can begin medication to help them detox from a drug, but Meieran still laments that there’s nowhere to direct that person once the immediate crisis has passed.
“You have no options,” she said. “If a person has a heart attack, they’re connected to a zillion different services that will follow up with them. They’ll get connected to a physical therapist, a congestive heart failure clinic."
That’s what the recovery world needs.
“At the very least, what’s needed is to start someone on medically assisted treatment and hand them off in a meaningful way,” she said “It would be amazing if there was a place with peer mentors who could help them connect to providers, treatment, housing."
She paused when she mentioned affordable housing, which seems always to be a barrier. Someone with a heart attack usually has a home to go back to, she said. And that makes their treatment more successful.
Increase Affordable Housing and Recovery Housing
Devarshi Bajpai, addiction services manager at Multnomah County, said having more affordable and stable housing in the community would free up residential treatment beds that should be reserved for people who need the highest level of care. Instead, those beds, which cost $6,800 a month, are largely occupied by people experiencing homeless, who are under some type of supervision for criminal activity, or who might have a psychological condition, but could still be served in a lower level of treatment if they had housing available.
“That’s not a cost-efficient way to address homelessness,” he said.
He suggested investing in more recovery housing, which has success rates similar to more intensive residential treatment beds. Recovery housing requires fewer staff and restrictions, making it less expensive to operate. Six months in recovery housing costs less than $10,000, compared to $27,000 for six months of inpatient treatment.
Central City Concern has more than 1,000 recovery beds in Multnomah County. Dr. Rachel Solotaroff, the agency’s chief executive officer, said clients who move into recovery housing after detox are three times more likely to complete treatment and 10 times more likely to seek primary care services. As a result, their total healthcare costs are less than half than those who don’t enter recovery housing.
Multnomah County, the City of Portland and Home Forward, the county’s housing authority, agreed last fall to add 2,000 more supportive housing units over the next 10 years, including new recovery housing made possible by closer collaboration with social services agencies and healthcare providers.
“If we bring together resources for housing, peer support, addiction treatment, we see not only better outcomes but also cost savings that we can reinvest,” Solotaroff said.
A Tremendous Opportunity
After the summit, Holton, Lines for Life’s executive director, didn’t waste time. That same afternoon he rallied presenters to focus on next steps, and asked them to submit proposals for tackling a series of ideas:
- Expanding medically-assisted treatment in jails
- Creating an Addiction Resource Connection Center
- Connecting emergency departments with treatment providers
- Connecting first responder connections with treatment providers
- Expanding the Law Enforcement Assisted Diversion program
- Creating an inventory of recovery housing needs
“We seized a tremendous opportunity today to improve policy around opioids and addiction and begin opening some of those pathways to recovery,” he wrote.
Multnomah County Chair Deborah Kafoury left feeling excited about the “real, tangible deliverables,” she said. She wants to work with emergency departments to get treatment options to patients, and she’d like to help the county’s addiction services division create a clearinghouse for treatment providers.
“Right now we offer one point of entry for people experiencing homelessness. But we don’t have anything like that for treatment,” she said. “There should be one place people can go for help.”
View Expert Presentations