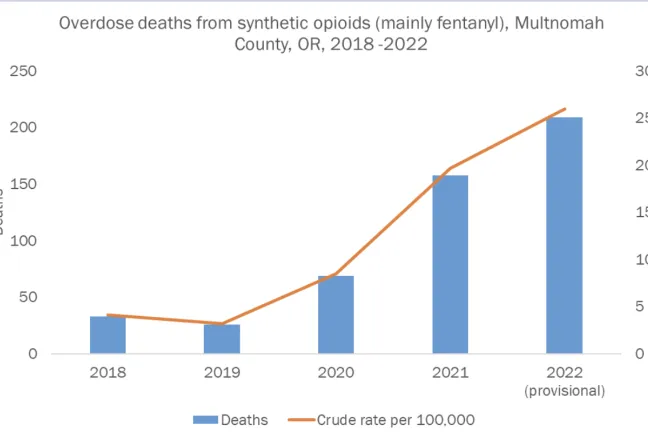
Overdose deaths from synthetic opioids have increased by 533% in Multnomah County from 2018 to 2022. The sharp upswing in overdose deaths, County health officials shared, reflects the rapid and radical change in local drug supplies towards fentanyl and other potent synthetic opioids which began in 2019.
Leaders from the Multnomah County Health Department presented to the Board of County Commissioners Tuesday, June 27, at the request of Chair Jessica Vega Pederson, who in May asked for a briefing about the local crisis around fentanyl use and overdoses, as well as the Health Department’s strategic response.
“I appreciate the intricate work that has gone into addressing the crisis within our Health Department as a whole,” Chair Vega Pederson said Tuesday. “We want to make sure that our investments and response to this crisis is going to yield the mitigation that the community really needs at this point.”
Health Department interim Director Valdez Bravo started the presentation by noting that the briefing was the first time the department’s divisions had come together in a public forum to talk about the current substance use crisis facing the country.
“In the Health Department, we understand the desire for tangible actions and solutions, and as community members, we share those desires and understand how living through these simultaneous crises impacts daily life,” Bravo said.
“We have the urgency. We sense the crisis and the gravity of the situation. We know that every day we don’t act, another life is lost.”
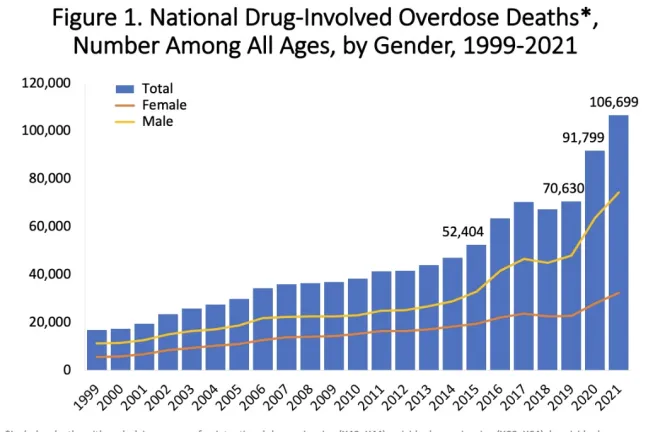
Synthetic opioids, like fentanyl, are dramatically more potent, more addictive and more deadly than heroin and other forms of opioids, Dr. Teresa Everson, the County’s interim health officer, explained. Drug overdose deaths, both unintentional and intentional, have had a sharp upward national trend over the past five to six years.
“It is so important to understand that what we’re experiencing in Multnomah County is not isolated,” she said.
“We are not alone as local public health leaders and elected officials grappling not just with how to keep up with the changing environment, but to get ahead of it. These conversations are happening across the nation.”
Everson went on to say that substance use interventions that historically have been successful do not have the same impact against substances at this level of potency and addiction. “These substances are not like anything we’ve seen in the last 40 years, including prior heroin epidemics, and are even harder to address with the buprenorphine-based medication-supported recovery services that have been expanding across the country.”
Between 2019 and 2021, overdose rates per 100,000 people in Multnomah County increased across all demographics, but were highest and rose the fastest in individuals over 30, Everson said.
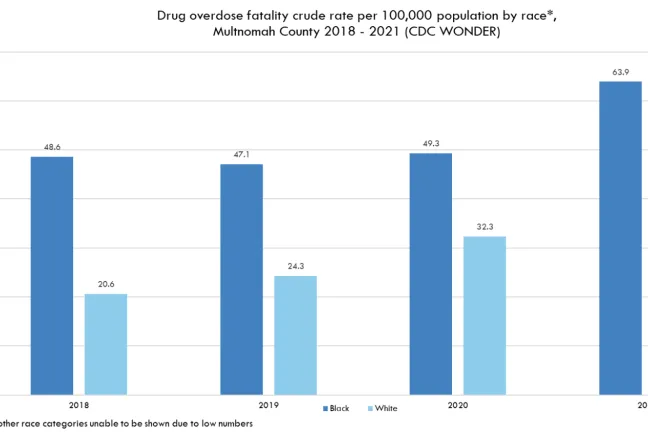
Overdose death trends are not just experienced disproportionately by age, but by race as well: A review of statewide data showed that American Indian and Alaska Native community members saw the highest rate of overdose death at almost 43 deaths per 100,000 people in 2020, nearly triple the statewide rate for non-Hispanic white individuals. Black and African American community members still experience overdose deaths at a rate 36% higher than white community members.
“This impacts everyone in our community. I know through my own personal extended family, friends and others that nobody is immune (from the fentanyl crisis),” Commissioner Julia Brim-Edwards said.
“There’s an urgent need for action and I look at the numbers and know that there’s a family in each one of those that is dramatically impacted by that.”
Polysubstance use
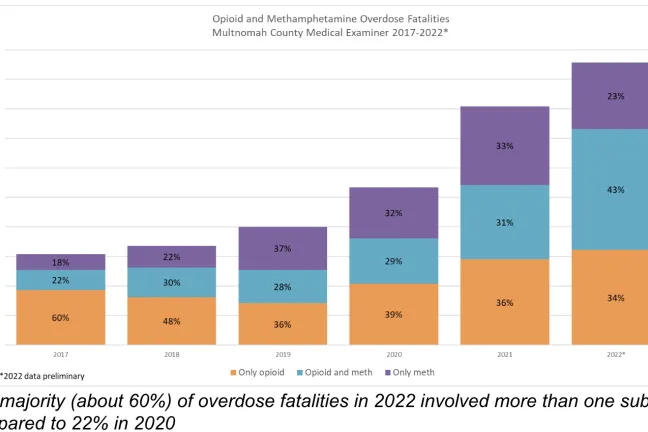
The second driving factor in the increase in overdose deaths is the growing number of people using both methamphetamine and opioids. Using more than one substance at a time dramatically increases the risk of overdose and makes care for the overdose more difficult. For those who do not overdose, the treatment of multiple use disorders and/or chemical dependencies is more complex.
“Many people often combine fentanyl with stimulants in an effort to balance the effects, hoping it will enable them to stay awake to accomplish tasks or stay safe,” said Kelsi Junge, a supervisor for the Harm Reduction Program.
“Mixing or alternating stimulants and downers is physically hard on the body and it increases the chance of overdose.”
Per data from the Multnomah County Medical Examiner’s office, the majority (about 60%) of overdose fatalities in 2022 involved more than one substance, compared to 22% in 2020.
“As long as our communities continue to grapple with the huge, systemic social challenges that drive dependence on illicit substances like trauma, economic insecurity and racism, people will continue to seek out methods to cope,” Junge said.
“Many people who are in chaotic stages of substance use and many of those who die of overdose are people that are trying to treat their physical or emotional pain.”
Health Department officials stressed that to successfully address fentanyl use in the community, other substances like methamphetamine and other forms of opioids must also be addressed.
“The hard truth is that the way we are currently set up, with the resources we have, the healthcare system and providers cannot compete with fentanyl,” said Ederlinda Ortiz, Corrections Health Transition Services program supervisor.
Health Department substance use response
While fentanyl and other synthetic opioids represent a newer, emerging threat, Bravo stressed that substance use is not a new issue and that Health Department programs have been connecting with and helping community members for years.
“Their long-standing role in our community is part of our success; they are trusted sources of information, resources and care,” Bravo said.
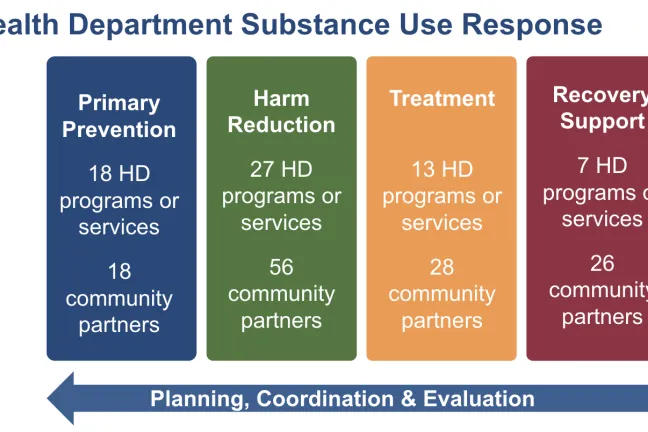
The Health Department’s substance use response, he said, can be divided into four categories: prevention, harm reduction, treatment and recovery.
Prevention
The primary prevention strategy for substance use introduces protective factors across critical periods and settings in a person’s life to mitigate against and decrease the risk of individuals engaging in substance use.
“Prevention programming gets at the root of factors that might drive substance use,” said Public Health Director Jessica Guernsey.
“By centering the understanding that the choices people make are based on the choices available to them, working at this level allows us to reduce ‘exposures’ that we know factor into lifelong health impacts.”
An example of the impact of prevention programming is the County’s Integrated Clinical Services Division’s policy change several years ago to reduce opioid prescriptions in their dental clinics by 97%. Guernsey explained how this change has resulted in significantly fewer youth being introduced to opioids in a clinical dental setting, which was historically known for advancing the use of opioid substances.
“Reducing the number of avenues that a person may access opioids is essential to preventing use in the first place,” Guernsey said.
The County’s school-based mental health programs have also started screening for substance use in the services they provide to more than 600 students.
Harm reduction
Multnomah County has been an innovator and leader in harm reduction practices for many years. According to Guernsey, harm reduction refers to policies, programs and practices that aim to minimize the negative health, social and legal impacts associated with drug use, drug policies and drug laws.
“The practice of harm reduction is grounded in justice and human rights, and focuses on positive change on working with people without judgment, coercion, discrimination or requiring preconditions to provide support,” Guernsey said.
The National Institute on Drug Abuse research, among others, has shown that harm reduction programs provide significant individual and public health benefits, including the prevention of deaths from overdoses and transmission of infectious diseases among people who use drugs and the larger community.
“I have been out talking to a lot of frontline workers and first responders and know the County’s harm reduction work is saving lives,” Brim-Edwards said.
Harm reduction services reduce emergency room visits and costly healthcare services. The services also offer a stigma-free environment to connect to recovery.
“Every week, my team and I spend hours providing services, care and support for people who are actively using substances of all kinds,” Junge said.
“We provide integrated harm reduction services, including access to supplies, safe disposal for used supplies, health education, wound care and HIV/STI testing, and sexually transmitted illness treatment.”
In Fiscal Year 2023, the Multnomah County Harm Reduction program saw 4,216 unique clients and distributed over 50,000 naloxone kits. Over 300 adults struggling with substance use disorder, houselessness or criminal justice risks were also connected to services.
Treatment and recovery
Multnomah County is unique because, unlike other counties that rely on state funding, treatment and recovery services provided by contracted community providers are paid from the County General Fund. The Behavioral Health Division has over 90 contracts totaling over $13.6 million annually that support a range of community-based programming, including culturally specific providers.
“When we first began to see routine use of synthetic fentanyl in 2018 and 2019, we started with the treatment approach that had historically worked for opioids and heroin,” said Anthony Jordan, addiction services manager for the Behavioral Health Division.
“It became clear the interventions were not effective for this substance. As a result, we’re in the midst of a pivot around the treatment and recovery services when it comes to addressing fentanyl.”
Board asks about capacity, other states’ response
Several commissioners asked questions about the healthcare system’s capacity to provide treatment and recovery services.
Commissioner Brim-Edwards brought up the limited capacity that keeps people who are ready for treatment services from accessing the help they need, asking how many additional treatment beds are needed “to meet this need so that we don’t have people saying ‘I’m ready for treatment’ and there’s no place for them to go?”
Dr. Jenny Tsai, Medical Director for the Behavioral Health Division, remarked that Oregon Health & Science University is working on a hospital bed dashboard that will increase efficiency for the current bed capacity.
“Sometimes it’s not a matter of beds, it’s a matter of coordination as to which level of care a client belongs to. I’m hopeful once that is developed, we can increase efficiencies within the system, whatever bed capacity there is,” she said.
Dr. Tsai also added that the Providence and Legacy hospital systems are actively developing additional detox beds that will become operational in the near future.
Commissioner Susheela Jayapal later followed that line of questioning.
“What’s our role in expanding capacity for outpatient services? Do we fund the additional contracts with providers?” she asked.
Jordan responded that even if the County could increase capacity by funding more providers, the lack of capital infrastructure, such as treatment facilities and beds, fragments the system of care and prevents the different aspects of the treatment and recovery system from being connected.
Chair Vega Pederson commented that for a long time, Oregon has ranked near the bottom in terms of the ability to provide treatment for the number of people who need treatment, and asked what the states that rank higher are doing differently.
“Who is actually providing those treatment beds, those services, whatever that looks like in other states? Where are the gaps happening? If it’s at the county level, I want to know that. If it’s at the state level…If it’s in the private insurers, the Medicaid providers, where are the gaps?”
Chair Vega Pederson also thanked the presenters for outlining the ongoing work throughout the Health Department to respond to the fentanyl crisis.
“The intensity of the impacts that we’re seeing on our streets now are unlike anything we have seen before,” she said. “I appreciate the way that the values of Multnomah County really shine through in the work that’s being done and how we are about meeting people where they’re at and providing people the path they need to recovery and stability.”